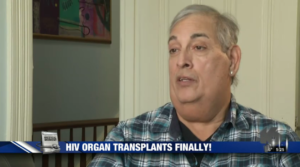
Reynaldo Garza, the first HIV-positive person to receive a transplant with an organ from someone with HIV, is healthy and living well a segment produced for NBC WNU shows.
Garza, who had the transplant two years ago, said that in the past HIV-positive patients who needed transplants were passed over for people without HIV.
“The prognosis is as good as for a person without HIV,” said Dr Peter Stock who performed the transplant.
Such HIV-to-HIV organ transplantations were illegal under federal and state laws written at the height of the AIDS scare in the 1980s. Those bans were repealed thanks in part to groundbreaking research by Stock that showed that transplants in HIV patients could be done safely and effectively.
Garza, a 59-year-old former florist who has been living with HIV for 20 years, became one of the first people in California to consent to receiving an HIV infected organ in November 2016, when he accepted a kidney from a deceased donor who tested positive for HIV.
“It was an easy decision for me,” said Garza. “I had been very sick for a long time. I was tired of going in for dialysis three times a week, for four hours at a time, sometimes at five in the morning if that was the only slot open. I already had HIV, I had hepatitis C, I had renal failure. I was like, ‘Yes, I'll sign anything. Just give me an organ.'”
Earlier this year a large-scale clinical trial was launched by the National Institutes of Health and could pave the way for more HIV-positive patients with kidney failure.
“We have an organ shortage crisis in this country and individuals living with HIV are disproportionately affected,” said Dr. Christine Durand, assistant professor of medicine at Johns Hopkins University and principal investigator of the study. The research will help determine whether the pool of HIV-infected organs is “safe and effective.”
If so, she says, it would benefit everyone awaiting kidneys.
“Every time someone with HIV gets an organ transplant they move everybody else up on the waitlist,” said Durand.
One estimate suggests there may be as many as 500 HIV-positive organs available every year. “But even if it's 10 a year,” said Stock, “that's taking 10 patients off the waiting list, and we need to use every organ that's out there optimally.”