A new injectable form of PrEP (pre-exposure prophylaxis) from ViiV Healthcare administered every two months has been shown to be 69 percent more … [Read more...] about Injectable Long-Acting PrEP Shown to Be 69 Percent More Effective at Averting HIV Infection Than Truvada
Body Conscious
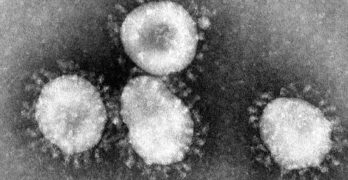
Coronavirus Poses Unique Risks for Many LGBTQ and HIV-Positive People: What You Should Know
As concern over the coronavirus mounts in the United States, it's understandable to be paranoid about what might happen, and LGBTQ people and people … [Read more...] about Coronavirus Poses Unique Risks for Many LGBTQ and HIV-Positive People: What You Should Know
The 2nd Person Ever to Be Cured of HIV Unmasks Himself
The second person ever to have been freed of the HIV virus has unmasked himself, a year after doctors announced they had successfully sent the virus … [Read more...] about The 2nd Person Ever to Be Cured of HIV Unmasks Himself
Why Gay Men Should Be Needy: WATCH
In a new video, Psychotherapist Matthew Dempsey urges you to speak up when your needs in a relationship aren't being met. Writes Dempsey: "Were you … [Read more...] about Why Gay Men Should Be Needy: WATCH
White House Considers China Flight Ban as Coronavirus Outbreak Worsens; 132 Dead; Americans Evacuated from Wuhan
The White House is considering suspending flights to and from China as the coronavirus outbreak worsens. The death toll stands at 132, up from 106 on … [Read more...] about White House Considers China Flight Ban as Coronavirus Outbreak Worsens; 132 Dead; Americans Evacuated from Wuhan
Calum Scott Shares Body Transformation: ‘I Always Yo-Yo with My Weight’
British singer-songwriter Calum Scott ("No Matter What", "Dancing On My Own") shared a body transformation photo on Instagram, acknowledging that his … [Read more...] about Calum Scott Shares Body Transformation: ‘I Always Yo-Yo with My Weight’
Maryland Company Claims to Have Cure for HIV/AIDS Through Gene Therapy, Expects Clinical Trial in January: WATCH
American Gene Technologies in Rockville, Maryland says it has submitted an application to the FDA for a gene therapy it claims eliminates HIV. CBS … [Read more...] about Maryland Company Claims to Have Cure for HIV/AIDS Through Gene Therapy, Expects Clinical Trial in January: WATCH
Scientists Discover First New Strain of HIV in Nearly 20 Years
Scientists have discovered HIV-1 group M subtype L, the first new strain of the HIV virus in 19 years during efforts to ensure that diagnostic tests … [Read more...] about Scientists Discover First New Strain of HIV in Nearly 20 Years
5 Tips for Surviving in an Increasingly Uncertain World
A recent study showed that North Americans are becoming less tolerant of uncertainty. The U.S. presidential impeachment inquiry has added another … [Read more...] about 5 Tips for Surviving in an Increasingly Uncertain World
Chris Hemsworth’s Workout Was So Hot His Shirt Burst into Flames: WATCH
It was thirsty Thursday for Chris Hemsworth, who shot this video to promote Centr, the fitness app launched by the actor and his team. Said … [Read more...] about Chris Hemsworth’s Workout Was So Hot His Shirt Burst into Flames: WATCH